In behavioral health, providers often encounter patients experiencing an acute psychological crisis that requires immediate attention. For these high-intensity sessions, two specific CPT codes — 90839 and 90840 — are used to bill crisis psychotherapy services. Understanding the appropriate use of these codes is essential for accurate reimbursement and regulatory compliance.
Therapists often face unique billing challenges. This overview breaks down key strategies for medical billing for therapists in private practice.
What Constitutes a Crisis?
A psychiatric crisis involves a sudden, intense disturbance in a patient’s emotional or psychological state. This may manifest as suicidal ideation, homicidal thoughts, severe panic attacks, psychotic episodes, or trauma-related distress. The provider must deliver immediate, focused psychotherapy to stabilize the patient and prevent further deterioration. These situations require immediate intervention, often with life-saving implications.
CPT Code 90839: First 60 Minutes
- Code: 90839
- Description: Psychotherapy for crisis; first 60 minutes
- Who Uses It: Psychiatrists, psychologists, PMHNPs, LCSWs, LPCs, LMFTs
Requirements:
- Face-to-face time must be at least 30 minutes but less than 74 minutes
- Involves urgent, unscheduled sessions
- Must include assessment, stabilization, and psychotherapy
- Medical necessity must be documented
The 90839 code can only be used when the provider determines that a patient is experiencing a crisis requiring immediate clinical attention. The crisis must interrupt the patient’s usual state and place them at risk, either mentally, emotionally, or behaviorally. Billing psychiatric evaluations requires careful attention to coding. Get clarity on initial session requirements with this guide on psychiatric evaluation billing.
CPT Code 90840: Add-On for Each Additional 30 Minutes
- Code: 90840
- Description: Add-on code for each additional 30 minutes beyond the initial 60 minutes
- Must be billed in conjunction with 90839
Example:
If a session lasts 90 minutes, you bill 90839 + 90840.
If a session lasts 120 minutes, you bill 90839 + 90840 x 2.
Providers must ensure they document clearly the extended duration and the clinical necessity for each additional 30-minute increment.
Documentation Must Include:
- Time spent face-to-face with the patient (start and end times)
- Nature of the crisis (e.g., suicidal ideation, violence risk, acute psychosis)
- Assessment tools used (e.g., Columbia Suicide Severity Rating Scale, BPRS)
- Stabilization techniques (e.g., safety planning, de-escalation, contacting support networks)
- Immediate treatment plan and referrals (e.g., ED transfer, safety contract, follow-up care)
Billing Scenarios
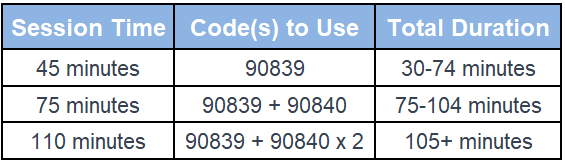
Properly choosing between these billing structures avoids under-coding for extended care or over-coding which leads to audits.
Ohio Mental Health Billing Tip:
Ohio Medicaid requires the provider’s NPI and rendering taxonomy code to match exactly — mismatches are a common reason for denials, especially for 90832–90837.
Check out our Ohio Billing Services page to keep your claims clean and compliant.
Payer Considerations
Medicare:
- Covers both codes when documentation meets urgency and time criteria.
- 90840 must not be billed as a standalone code.
- Telehealth coverage often includes these codes with appropriate modifiers.
Commercial Insurers:
- Policies vary; some require pre-authorization or limit the number of sessions.
- Confirm medical necessity, and verify benefits before the session.
Medicaid:
- Coverage is state-specific. Some Medicaid programs may cap usage of 90839 or require state-specific modifiers. Always verify guidelines with your local Medicaid agency.
Common Mistakes to Avoid
- Billing 90839 for routine sessions: This code is for true crises, not longer or intense therapy sessions.
- Omitting start and end times: This can trigger audits or denials.
- Failing to document risk levels or assessments: Insufficient justification for crisis coding.
- Billing 90840 without 90839: 90840 cannot be used independently.
Real-World Insight
At Global Tech Billing LLC, we’ve helped practices reduce denials by 40% simply by training staff on the proper use of 90839/90840. For example, a mental health clinic in New Jersey previously misused 90839 for every intake session. After we provided a targeted training session, they corrected their usage saw an 18% increase in approved reimbursements, and avoided potential payer audits. Just starting with testing services in private practice? Make sure you’re coding properly with this guide on
psychological testing services.
Why Correct Coding Matters
Crisis intervention services are time-consuming, high-stress, and critical. Providers must be appropriately reimbursed for these vital services. Incorrect coding leads to delayed payments denied claims, or worse, compliance audits. By ensuring proper documentation and code use, practices protect their revenue and reputation.
Accurate billing for crisis intervention not only ensures compliance but also upholds the integrity of mental health care delivery. It also allows providers to allocate resources efficiently and improve service quality during emergencies.
Final Thoughts
Crisis intervention demands clinical skills and responsive documentation. Understanding the nuances of 90839 and 90840 empowers mental health providers to deliver urgent care without compromising revenue. These codes reflect the unique and challenging nature of crisis therapy — getting them right is not optional, it’s essential. For official guidelines on crisis psychotherapy billing, you can refer to CMS – Psychotherapy for Crisis.
If you’re unsure whether your crisis billing is optimized, Global Tech Billing LLC offers complimentary audits to ensure you’re not leaving money on the table. We’ve helped providers improve revenue and stay audit-ready — and we can help you too.
Frequently Asked Questions (FAQs)
1. Can I use 90839 for telehealth sessions?
Yes, if the crisis criteria are met and payer policies allow it. Always include proper modifiers such as 95 or GT.
2. Can 90839 be used during a scheduled session?
Only if the session escalates into a crisis requiring intensive intervention. This shift must be documented with justification.
3. What if a session lasts less than 30 minutes?
Do not use 90839. Consider a standard psychotherapy code such as 90832 or 90834, depending on actual session length and complexity.
4. How often can I bill 90839?
There’s no hard limit, but frequent use may trigger payer scrutiny. Justify frequency with clinical notes, risk levels, and treatment rationale.
5. Does 90840 require its documentation?
Not separately, but documentation must show the total face-to-face time, what was accomplished during the extended session, and why it was clinically necessary.
6. Can I bill 90839 alongside other codes?
Generally, no. You cannot bill 90839 with E/M or standard psychotherapy codes for the same visit unless they are distinct and separately identifiable services — and even then, strict rules apply. Always review payer guidelines.
7. Is there a difference in reimbursement between 90839 and standard psychotherapy?
Yes. 90839 generally reimburses higher due to its intensity and urgency. Rates vary by payer and location but typically range from $150–$220 for 90839, with each 90840 add-ons reimbursing an additional $70–$100.
